James P. Allison (Texas, United States, 1948) earned a BS in Microbiology at the University of Texas, Austin, where he went on to complete a PhD in Biological Science in 1973. He later spent twelve years at the University of California, Berkeley, where he was Professor of Immunology and Director of the Cancer Research Laboratory.
After stints at the Memorial Sloan-Kettering Cancer Center and Cornell University, and as an investigator with the Howard Hughes Medical Institute, in 2012 he joined the team at Texas University’s MD Anderson Cancer Center, where he is currently Chair of the Department of Immunology, Vivian L. Smith Distinguished Chair in Immunology, Executive Director of the Immunotherapy Platform, Deputy Director of the David H. Koch Center for Applied Research of Genitourinary Cancers and Co-Director of the Parker Institute for Cancer Immunotherapy.
He has also kept up a thirty-year association with the National Institutes of Health, where he chaired the Experimental Immunology Study Section and has served on expert panels on gene therapy, as well as organizing a think tank on cancer biology.
He sits on the editorial board of Developmental Immunology and Journal of Clinical Investigation and is a former reviewing editor of Science. The holder of six patents, he is also the co-founder, with his wife and scientific colleague Padmanee Sharma, of clinical stage immunotherapy company Jounce Therapeutics.
Since receiving the BBVA Foundation Frontiers of Knowledge Award (2017), he has gone on to win the Nobel Prize in Medicine jointly with Tasuku Honjo (2018).
In 2011, Allison’s efforts led to the approval by the U.S. medicines agency (the FDA) of the first anti-cancer drug that works by activating the immune system, for the metastatic melanoma indication. The treatment would exceed all expectations, with around 20% of patients still living ten years later. The drug in question – ipilimumab – has produced a “complete paradigm shift” in the way medicine approaches cancer therapy, explains jury member Lélia Delamarre, Group Leader in the Cancer Immunology Department at biotech company Genentech.
Several drugs based on Allison’s principle have since been approved, seeking to boost the percentage of melanoma patients who can benefit from immunotherapy. Effectiveness has also been found for this line of treatment in lung, kidney, bladder and head and neck cancers.
Immunotherapy works by mobilizing the system’s natural defenses to combat and eliminate specific cancer cells. Over the years, various runs had been made at the strategy, but without success until Allison stepped in. The insight which would transform the therapeutic landscape was his discovery, in the mid-1990s, of a key mechanism in the functioning of the immune system T cells responsible for fighting tumor cells.
Allison and his group had determined that mobilizing these cells required the activation of two specific cell “switches”; yet this was not enough in itself to defeat the cancer cells. It was then that Allison proposed that a third signal must exist, with the ability either to boost the activity of these T cells or, conversely, block their function – the immune system is tightly regulated by positive and negative signals to stop it turning against the host body. Allison eventually “characterized a molecule called CTLA-4, which is displayed on the surface of T cells, and showed that it normally acts as a brake on this function,” in the words of the citation.
The next step was to block this third signal, doing what jury member Robin Lovell-Badge of the Francis Crick Institute describes as “taking a foot off the brake” of the immune system. The T cells can then act unhindered against the cancer cells that are their target. Mouse trials of this strategy produced promising results, but the scientific community was not immediately convinced.
Allison recalled this period in a phone conversation yesterday after hearing of the award: “This skepticism was a reaction to the excess optimism of the early days of immunotherapy. At the start of the 1960s, people started talking about a new system destroying cancer, but the fact is that it only worked in mice. What happened I think is that people rushed in to do things without really understanding the underlying mechanism. They didn’t realize that there are these negative signals built into the immune system, which are there to protect us. There were a lot of failures and people just gave up, insisting it was all hype.”
The good results of clinical trials in humans, initiated in 2001, not only proved Allison right, but also inspired many other researchers to start searching for new immune system brakes or checkpoints. Immunotherapy is now one of the most active areas in oncology.
Among its advantages is that the response is lasting and may even lead, in some patients, to remission of the tumor, because the immune system will recognize the cancer cells if they reappear. Also, as Allison points out, “we don’t tackle the cancer directly, we get the immune system to attack it,” meaning immunotherapy can be effective against multiple tumors. A third advantage is that treatments generally have fewer side effects.
Allison, however, is the first to warn that immunotherapy is no one-stop solution: “We’re not going to be able to cure all cancers,” he admits. “But I think that in future immunotherapy will be a part of all cancer treatments, in combination with chemotherapy or radiation. I am optimistic that we will learn the right things to put together to cure a majority of patients, maybe even reaching from 60% to 90% of cases in some kinds of cancers.”
Despite the good news, above all in cancers like melanoma that have so far proved largely intractable, immunotherapy still only works in a given percentage of patients. Some tumors manage to block the immune system or even slip by it unnoticed, and patients’ treatment responses are at times unpredictable. That’s why Allison insists on the need for more basic research: “The bottom line is we don’t really know why the treatment doesn’t work in all patients. A lot of people are looking for some sort of marker or sign so we can predict who is going to respond or not. But we just don’t know. All the more reason to keep on doing the basic work.”
Allison defines himself as a basic researcher, or at least that is how he started out: “I had a personal interest in cancer, because I lost my mother when I was a small child, and later my brother and two of my uncles. But I first wanted to figure out how T cells worked, so I could maybe apply the lessons of this basic research to come up with a cancer therapy. I think you first have to know basic science. Without that fundamental biology you do not have a rational basis for treating cancer. I always had possible cancer applications in the back of my head, but the priority has to be to do the best science you can, not necessarily with a specific goal in mind. That’s what I always tell my students.”
Despite this, Allison has had the rare privilege of meeting people who have benefited directly from his work: “One of the greatest moments of my life was seeing a woman who had been told she was going to be dead in a few months, and over 15 years later she is still alive and has two children. That motivates me to do all I can to get these therapies to work better. It’s pretty rare for a basic scientist to get to see the application of their findings. I was lucky enough to have that experience.”
Allison is now working with his wife and colleague at MD Anderson, Padmanee Sharma, on what they call the “Immunotherapy Platform”: “We are currently involved in about a hundred clinical trials to analyze the effectiveness of these treatments. We are studying patients’ tissues pre- and post-treatment to find situations where it works and where it doesn’t, trying to probe the molecular details to understand where treatments may be falling down.” All in all, the new laureate sees reasons to be hopeful: “we are not going to wipe out cancer, but we’ll get a lot better at fighting many kinds.”
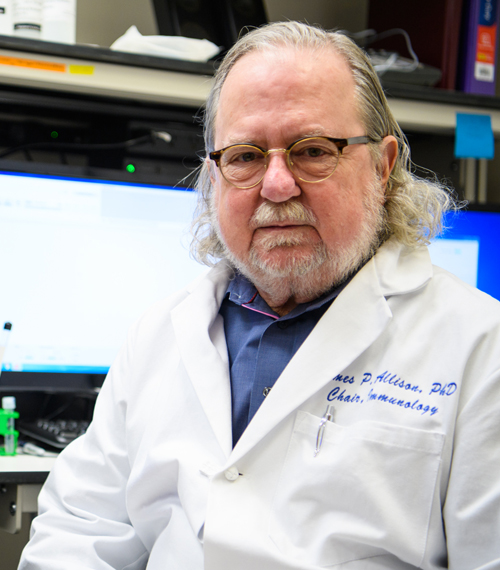
Photo © University of Texas, MD Anderson Cancer Center